
Are Prior Authorizations Driving Your Staff Crazy?
If they are, then you’re not alone!
Prior authorizations are a nature of our business to ensue, or at least hopefully, we get paid for the services our physicians provide to their patients. Most of us have been medical practice executives for years and have seen the burden to get paid become more and more difficult. It’s like the insurance payers have a different play book than they gave us to help with claims processing.
I was recently reviewing claim denials and noticed a few claims were denied due to missing prior authorization. In my opinion, the patient should not have been seen by the physician, unless it was an urgent or emergent visit, without having the authorization on file at the time of the appointment. Furthermore, according to Health Payer Intelligence, prior authorization issues contribute to 92% of care delays. Just think about the impact on a cancer patient’s stress level, and the physician and staff, when they’re told about a delay in their treatment plan due to a prior authorization issue. In some cases, the insurance payer may recommend an alternative, less expensive, therapy instead of the physician’s first choice for treatment. There’s a good chance that we all have a personal story about a family member or friend whose treatment was delayed.
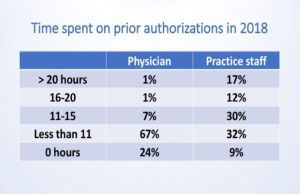
In a recent Medical Economics article, physicians were asked several survey questions and the results should not be surprising to anyone regarding the amount of time the physician and staff spend on prior authorizations is staggering.
Athena Healthcare prepared a white paper titled “3 Ways to Take the Burden Out of Prior Authorizations”, which is worth reading. The paper addresses strategies to help overcome problems with obtaining prior authorizations by ensuring your staff is knowledgeable of the various payer requirements, to include tracking the status of the prior authorization. The staff should work with the payer if they notice a trend of claim denials due to prior authorization not being received. Additionally, the billing team should be notifying the practice manager as soon as they begin to notice a trend with denied claims. According to Patient Engagement IT, 36% of physician survey respondents indicated they hired a dedicated staff member to handle prior authorizations. I recently did an online search of three salary websites to obtain the pay for a Referral Coordinator, and the average pay in San Antonio was $13.51 per hour, or slightly more than $28,000 per year.
The good news! There could be some relief in sight if Governor Abbott signs Senate Bill 1742 that was sent to him on 5/28/2019. At the time this article was written, Governor Abbott has not signed Senate Bill 1742. The TMA sent a Call to Action just before the Legislative Session ended. Online research on 6/5/2019 indicates Governor Abbott has not signed Senate Bill 1742, so there’s still time for your physicians to contact the Governor to sign the Bill.
Let’s hope the prior authorization issues resolve soon so that our staff can spend more time on patient care than administrative hassles. I would love to hear your feedback… please e-mail me at tom@concordispm.com. Thank you for reading the article.
References:
https://healthpayerintelligence.com/news/prior-authorization-issues-contribute-to-92-of-care-delays
https://www.athenahealth.com/sites/ahcom/files//authorization_management_whitepaper.pdf
https://patientengagementhit.com/news/91-of-docs-say-prior-authorization-delays-patient-care-access
https://www.indeed.com/salaries/Referral-Coordinator-Salaries,-San-Antonio-TX
https://www.payscale.com/research/US/Job=Referral_Coordinator/Hourly_Rate/954586ea/San-Antonio-TX
https://www.simplyhired.com/salaries/search?q=medical+referral+coordinator&l=San+Antonio%2C+TX



No Comments